Hypnotherapy For Neuropathic Pain – What Can Be Done For Neuropathic Pain?
 Neuropathic pain runs the gamut depending on whom you ask. To some people, their days are ruined as a result of the excruciating pain they feel on a day-to-day basis. To others, the pain can be annoying, and they just learn to deal with it. Many others feel numbness in their feet and lower limbs. Ultimately, everyone is looking for some type of treatment to alleviate the pain which could include anything from exercise, changing daily routines, incorporating hypnotherapy for neuropathic pain, in addition to other techniques so that the pain could ultimately subside.
Neuropathic pain runs the gamut depending on whom you ask. To some people, their days are ruined as a result of the excruciating pain they feel on a day-to-day basis. To others, the pain can be annoying, and they just learn to deal with it. Many others feel numbness in their feet and lower limbs. Ultimately, everyone is looking for some type of treatment to alleviate the pain which could include anything from exercise, changing daily routines, incorporating hypnotherapy for neuropathic pain, in addition to other techniques so that the pain could ultimately subside.
What is the best way to measure pain? Everyone has different thresholds so there is no tried and proven test or device on the market that can accurately measure pain. As a result, doctors pay tons of attention to how the patient describes his or her pain. Since the pain varies from levels of dullness to excruciating, the physician is looking for any clues that can help identify patients’ level of pain. These clues can then be documented in a patient’s pain history when conducting an initial exam.
The patient can also experience neuropathic pain if they have visible lesions or other calamities associated with the nervous system. Obviously, someone with this type of pain would vary greatly from another that experiences pain from time to time. As a result, neurologists are constantly developing trials to provide pain relief. While prescription drugs can be seen as the first choice when dealing with so many variables, doctors are also open to collaborating with the alternative health communities since there is not a one size fits all treatment for individuals.
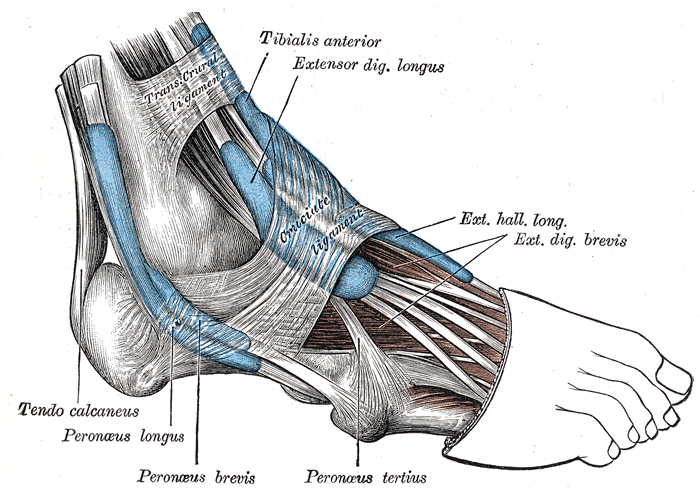
What Causes Neuropathic Pain In Feet?
Is it possible to provide the same treatment for two separate patients that have the same pain? For example, the numbers continue to increase with people that have diabetes. The complications from the high blood sugar would lead to numbness, as well as various levels of pain in a person’s lower extremities. The current statistics point over twenty-five percent of patients with diabetes that complain about the pain in their feet and legs. New neuropathy treatments are being studied to meet the growing demand.
One test, that has grown in popularity to measure pain, is the nerve conduction velocity test. An electric current is used on the skin. impulses and nerves are studied to measure how quickly they move along healthy versus damaged nerves. This test is also used so that other muscular disorders can be excluded. Ultrasound is another strategy that is used to identify pain in patients. This is also popular since the patient does not have to go under anesthesia, and they can be awake during the process.
The American Medical Association approved the technique of hypnosis in 1958 as a complement to medication given to treat pain. Hypnosis allows an individual to relax while giving suggestions by a clinical hypnotherapist. Suggestions are given to ease the patient’s mind to help them cope with excruciating pain. The theory suggests that pain relief occurs because the nervous system is slowing down pain impulses in the body.
In 2008, scientists at the National Institute of Health sought to test the theory of using virtual reality hypnosis (VRH) as a way to combat pain in patients that had tried all other treatments but had not experienced success over a period of five years. The trials ran for over six months with over 33 sessions where their pain levels were being measured. Pain ratings dropped after each session of the virtual-reality treatment. In some cases, the patient didn’t experience any pain at all after these treatments. The findings also pointed out that the pain reduction was not long-lasting. Each patient had to continue with hypnosis sessions to keep the pain at a tolerable level.
Self-hypnosis has been recommended as a way to deal with pain for the last 20 years within the scientific community. The level of self-hypnosis varied with the patients as some listened to general tape recordings while others had individually based hypnosis sessions. Research findings have been unable to properly identify which tactic is better concerning the standard tapes that could be given to anyone versus individualized recordings. The other sticking point is the actual number of times that a person has to listen to a hypnosis session in order for it to be effective. While the findings could not identify an actual number, the overall agreement was that the patients who continued to listen and practice hypnosis had longer-lasting effects with regards to dealing with pain.
The decision to measure pain can present a conundrum for hypnotherapists who traditionally practice Emile Coue’s 3 laws of suggestion and the principle of prestige.
Coue’s 1st law – the law of focused attention: what one focusses upon, increases. When focusing upon saving money, saving increases, and when focusing upon spending money, spending increases. Therefore when asked “how is the pain today?” the patient’s focus is drawn towards the pain, which therefore also increases. While working as a quality manager at a private surgical hospital in wellington, New Zealand in 2010, hypnotherapist Andrew Hardwick DipClinHyp, DipAdvHyp, DipM, CHt, MIACT, changed the nursing practice of asking a patient to indicate their pain levels on a “pain scale” of 1-10. It was replaced by a “comfort scale”, again from 1-10. The effect of asking “how comfortable are you today” resulted in a measurable decrease in the number of analgesics prescribed. This simple act of changing words to influence focus made a difference in the quality and nature of the patient’s hospital stay. Footnote; the “comfort scale” was later implemented across all hospitals in the organization.
Coue’s 2nd law – the law of dominant effect: an effect is an emotion, and whichever emotion is dominant at the time will determine what actions will be taken. Building upon Coue’s 1st law, if a patient perceives pain they will behave differently to if they perceive comfort. Thus, a person perceiving pain may believe they need analgesics, whilst a patient perceiving comfort may not. This is what happened in the above scenario.
Coue’s 3rd law – the law of reversed effort: this law states that when one believes one cannot do something, the harder one tries to do it, the harder it is to do. So, when a patient believes they cannot live another day in pain, the harder they try to not live another day in pain, the harder it is to not live another day in pain, and so they do live another day in pain. This is psychologically a double-edged sword. On the one hand, it can stop many patients from trying to avoid living another day, but on the other hand, it reinforces their belief that every day they do life will be in pain. Coue’s 1st & 2nd law of suggestion can be used by hypnotherapists to turn this around. This is done by turning this on its head, namely, when one believes that one can do something, the harder one tries not to do it, the harder it is to not do. In essence, once the patient has learned that they can live a day in comfort, the harder they try to not live a day in comfort, the harder it will be for them to not live a day in comfort.
The principle of prestige: when a person “looks up” to someone in authority, a position of prestige, it is easier to accept the suggestion from them. This too is a double-edged sword. If a doctor or nurse says “how is the pain today?”, it implies to the patient that the authority figure expects them to have pain, so they respond by finding some. Therefore, if the same doctor or nurse were to ask “how comfortable are you?” the same patient will most likely respond by accepting that this authority figure expects them to feel comfortable, and so will find comfort. This will impact upon all of Coue’s laws above.
Coue’s laws of suggestion and the principle of prestige all work consistently when applied scientifically. They work because all our sensations, including pain, are based upon perception rather than reality. For example, we do not see with our eyes and we do not hear with our ears. In reality, the eyes and ears are merely tools used to collect sensory input from various sources. The input is then sent to the brain for interpretation, and we give them a name such as “pain” or “comfort”. Clinical hypnotherapy can be used to reprogram the patient’s thoughts to interpret sensations as “comfort” instead of “pain”.
Historically, the use of hypnosis for pain control can be traced back several centuries. For example, in this reference from wikipedia.Org, Dr James Braid (19 June 1795 – 25 March 1860) was a Scottish surgeon and “gentleman scientist“. He was a significant innovator in the treatment of club-foot and an important and influential pioneer of hypnotism and hypnotherapy. He is regarded by many as the first genuine “hypnotherapist” and the “father of modern hypnotism”.[1] Dr Braid did hundreds of surgical procedures using only hypnosis for anesthesia
Andrew Hardwick, also has personal experience of self-hypnosis for pain control and anesthesia. In 2011, he suffered a broken leg during a martial arts accident. Metal retaining screws were used to stabilize the right ankle. Months after the accident, the screws needed to be removed. He decided to use self-hypnosis for the procedure, rather than have anesthetic. After a fight to secure the legal right to have an operation without anesthetic, the operation was done. He walked into the operating area, laid on the operating table, got into position, and put himself into hypnosis. When he gave the surgeon a pre-agreed signal, a nod, they cut into his leg, took out the metal and stitched his leg up. He said that he felt no pain at all! Within 10 minutes was having lunch on the post-surgical unit, and an hour later, went home. Without the need of anesthetic and said that he needed no analgesia and no extended, potentially expensive, hospital stay either. Hypnosis for pain control is that powerful!
It is important to understand that a growing number of people are dealing with neuropathic pain and have pain that is affecting nerves as well and muscles. Since that is the case, exercise alone will not repair motor nerves that are damaged which affects muscle movement. While symptoms of pain vary greatly among patients, it is recommended to speak with a doctor immediately to discuss all the issues. The doctor may also offer alternative methods like hypnotherapy to complement any medication that is given.
An explosion of interest in the applications of hypnosis for clinical problems, especially pain, has led to a wide accumulation of research on hypnosis as a viable, beneficial supplement to treatment protocols. Over the past two decades, published controlled trials have confirmed that hypnosis treatments are effective for reducing daily pain intensity, increasing activity level, and improving mood and sleep quality in individuals with chronic pain. Moreover, evidence also suggests that hypnotic procedures can increase the beneficial effects of other treatments, such as cognitive-behavioral therapy (CBT). Based on these findings, there is a lack of practical resources in the field that offers recommendations for incorporating hypnosis and hypnotic protocols into treatment for pain management. This therapist guide fills this gap by distilling the techniques empirically validated by these clinical trials into one comprehensive, user-friendly volume. Organized into three parts, Hypnosis for Chronic Pain Management summarizes the findings from research, examines the effects of hypnosis on pain, and provides step-by-step instructions for performing hypnotic inductions and making hypnotic suggestions. Designed to be used in conjunction with the corresponding patient workbook, this unique therapist guide is written for clinicians who treat patients with chronic pain and who wish to incorporate hypnosis and hypnotic procedures into their treatment protocols, or those clinicians who already have training in clinical hypnosis and hope to acquire the skills needed to apply it to pain management. “An excellent blueprint to understanding pain and the fundamentals of how hypnosis combined with CBT can offer pain amelioration. Perfect, even for uninitiated practitioners who wish to use empirically based scripts.”–Jeffrey Zeig, Ph.D., The Milton Erickson Foundation “Pain can too easily enslave people, holding them captive in many different ways. It is a liberating theme of empowerment that echoes throughout Dr. Jensen’s work: he empowers clinicians to work more knowledgeably and skillfully with people who suffer painful conditions using his therapist guide, and he encourages the suffering individual to break free from pain’s grip with the practical pain management skills taught in his workbook. Dr. Jensen’s vision for the many ways hypnosis can help reduce the debilitating effects of painful conditions is fresh, inspiring and should be regularly integrated into every pain management program.”–Michael D. Yapko, Ph.D., Clinical Psychologist and author of Trancework: An Introduction to the Practice of Clinical Hypnosis (Third Edition) and Treating Depression with Hypnosis


